Blood in the stool could be a minor nuisance or a sign of some serious medical disorder, but it should not go unchecked. Rectal bleeding may not necessarily result in a life-threatening, terrible disease, but it could be something that could result in severe complications and should be accurately diagnosed by an expert gastroenterologist. The award-winning specialists at Manhattan Gastroenterology use the latest technological advancements and research to find out why you are having bloody stools and develop personalized treatment plans that lead to long-term relief and wellness. The gastro doctors also look for any specific conditions that may be leading to the presence of blood in the stool and help you manage them to prevent any more episodes.
Bleeding anywhere along the digestive or gastrointestinal tract, from the mouth to the anus, is not normal and should be taken seriously. However, it may not be alarming and could be managed with lifestyle and dietary changes and medications prescribed by your healthcare provider.
The longer the blood is present, the darker it will be by the time it reaches the toilet. Bright red blood usually indicates it is coming from the lower portion of the GI tract, either the colon, rectum, or the anus.
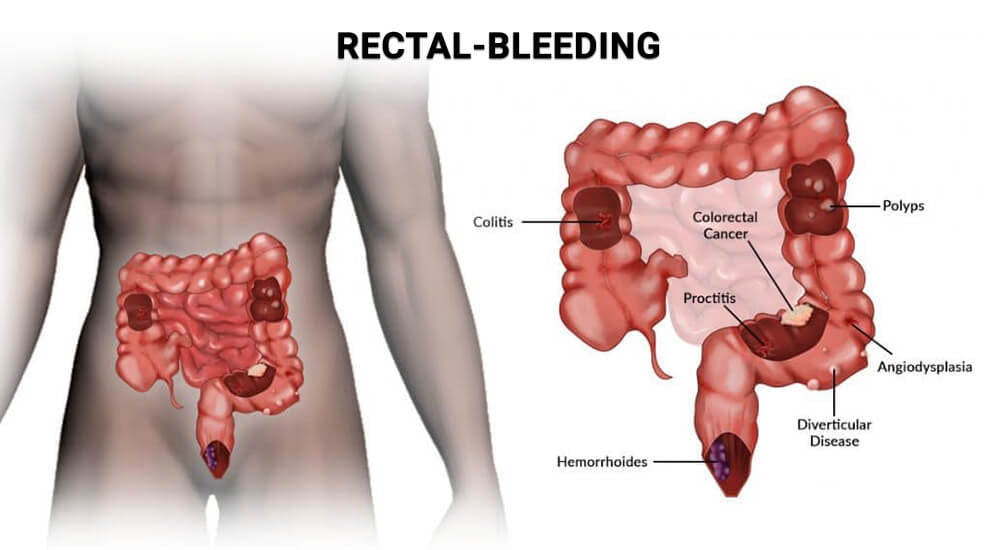
Here are some of the most common gastrointestinal issues that can be the reason behind bright red blood in your stools.
Hemorrhoids
Hemorrhoids are swollen blood vessels or veins inside or outside the anus and most likely cause bright red blood in your stool. These veins are harmless, but they are fragile and can bleed. Hemorrhoids inside the rectum are internal hemorrhoids, while those at the anus are external hemorrhoids. They are often caused by common issues such as:
- Chronic constipation
- Straining during bowel movement
- Lifting heavy objects
- Frequent anal intercourse
- Obesity
- Childbirth
All these factors put strain or pressure on the rectal area, which results in bleeding. Hemorrhoids are not dangerous or need a rush to the emergency room. Many times they even resolve on their own without needing any treatment.
The occasional blood you see on the tissue paper or in the toilet bowl is not something to worry about, but if they become painful, bleed too much, or begin to affect your normal life, seek medical help. Multiple treatment options are available to heal or remove hemorrhoids.
Anal Fissures
An anal fissure is a split or tears in the skin around the anus. It is an abnormality of the anus that can lead to abscess and form pockets of infection which cause bleeding. They occur when you suffer from constipation frequently and have to pass a hard stool. The extra pressure of the bowel movement can split the skin sensitivity. An anal fissure can make you bleed when you use the bathroom and feels a burning sensation during the bowel movement.
Signs of anal fissures include:
- A visible crack in the skin surrounding the anus
- Pain during and following bowel movements
- Blood in the stool
- Itching or irritation around the anus
Anal fissures are sometimes confused for hemorrhoids too, due to similarity in symptoms. Small tears usually go away on their own over time and do not require treatment. However, if you suffer from persistent constipation and anal fissures, it is important to seek medical help. These fissures may be a sign of an underlying issue that is causing their development and may lead to complications.
Anal Abscesses
An abscess is a deposit or small pocket of pus that develops in the lining of the anal canal, usually as a result of bacterial infection. An anal abscess can have many different causes. It is caused by the blockage of a gland. When these glands become clogged, they become inflamed and infected, forming abscesses. They can also occur from an anal fissure tear in the canal that becomes infected and sexually transmitted infections.
Symptoms of anal abscesses include:
- Skin irritation around the anus
- Discharge of pus and blood
- Tenderness and swelling
- Constipation or pain associated with bowel movements
- Fever
- Chills
- Fatigue
Abscesses often appear as a painful boil-like swelling near the anus. They rarely go away on their own and require medication and surgery to open and drain the abscess to relieve pressure and discomfort and prevent bleeding.
Diverticular Disease
This disease results from a weakness in the bowel wall that leads to the formation of small pouches or diverticula. They can show up anywhere in your intestines and protrude through the walls of your bowels, causing bleeding and infections. When these pouches get infected, they can cause symptoms like abdominal pain, fever, and a sudden change in bowel habits.
People often live their entire lives with diverticula and do not have any symptoms. Bright red blood in your stools is an indication of diverticular disease. If these diverticula become inflamed and infected, they can cause bleeding, fever, and persistent pain for several days with a sudden change in bowel habits.
If you suffer from chronic diverticulitis, inflammation and infection may go down but do not clear up completely. Over time this inflammation can lead to bowel obstruction that can further deteriorate the symptoms especially bleeding, and make you feel sick.
Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease is chronic inflammation, swelling, and pain in the small and large intestines that often causes bright red blood in stools. It includes two types of conditions, Crohn’s disease, and ulcerative colitis. Crohn’s disease can affect any part from the mouth to the anus. It is a condition where you develop patches of swelling in the digestive tract. It can often involve the deeper layers of the digestive tract.
In ulcerative colitis, the inflammation and sores are mainly in the large intestine or colon and rectum. People with IBD might experience fever, diarrhea, abdominal pain and cramping, intestinal blockages, and rectal bleeding. Long-term rectal bleeding can lead to low levels of red blood cells, which makes it crucial to get yourself checked if you notice blood in your poop.
IBD can be debilitating and even leads to life-threatening complications if you do not seek timely treatment. Medications and surgery are the best ways to manage your symptoms.
Polyps
Polyps are unusual growths on the inside wall of the colon. Most of them are benign or non-cancerous and do not cause any painful symptoms. However, polyps can bleed, particularly the large ones that get irritated. Colon polyps may occur due to changes in the mucous lining of the colon. There may be no specific reason behind them. They could be a result of genetic changes, or some underlying condition such as IBD.
They can appear as a mushroom growing out of the side of your bowel. Bleeding polyps can lead to bright red blood in your stool which is scary if it persists. In some cases, polyps can turn into cancer if they are not treated timely. It is necessary to have rectal bleeding related to polyps checked by a doctor as it could also be a sign of colorectal cancer. Polyps can be removed during a colonoscopy, or your doctor can get rid of them through surgery.
Ulcers
Ulcers are erosions of the lining of the intestinal tract. When the amount of digestive fluids in the intestines is out of balance, the stomach acids can etch away the protective layer of mucus, damage the lining of the digestive tract and cause open sores or ulcers. They usually occur in the stomach and small intestine, due to which blood in the stool appears dark or tar-like by the time it reaches the stool.
Some people have no symptoms, and their ulcers lay quiet for years. Others may experience discomfort or burning pain and heartburn after they eat. If the ulcer has eroded or damaged an artery, it will result in rapid bleeding, which appears as bright red blood in your stool. It is serious, and you must contact your doctor immediately as excessive loss of blood can lead to weakness, dizziness, and even life-threatening situations.
If you are seeing blood in your stool, it is essential to see a healthcare provider before things turn bad. The sooner you consult a gastroenterologist and begin treatment, the better chances you have of preventing the disease or disorder from advancing and creating complications.
What to Do if You Are Having Bright Red Blood in the Stool?
The best thing to do if you are noticing blood in your stool is to monitor your symptoms and pay attention to any unusual signs you are having. Rectal bleeding is a serious matter and should not be taken lightly. If you are not sure about what is causing bloody stools, schedule an appointment with your healthcare provider for evaluation and diagnosis.
The doctor may ask the following questions regarding your condition:
- Was the blood in the stool, toilet bowl, or toilet paper?
- Was the blood bright red or dark red?
- How much blood did you see? Even a drop of blood in the toilet bowl can turn all the water red
- Do you have to strain to pass the stool?
- How frequently do you have bowel movements?
- Do you have other symptoms?
- When did you last go for colon cancer screening or colonoscopy?
- Do you have a history of polyps or a family history of polyps?
- Do you suffer from hemorrhoids?
Your answers will help the doctor figure out what you may be going through and make an accurate diagnosis. You should also tell your physician if your rectal bleeding does not stop, you see large amounts of blood, or your stools are foul-smelling with a coffee-grain appearance. The doctor will take your medical history and recommend tests, including a physical exam, endoscopy, colonoscopy, and other investigations to locate the site of bleeding and its causes.
If you notice bloody toilet paper or the water in the toilet bowl turns red after your bowel movement, consult your doctor to learn what may be causing it and if it is a warning sign of some health condition. Experienced and board-certified gastroenterologists at Manhattan Gastroenterology diagnose the causes of blood in the stool to determine which treatment will work best for your gastrointestinal health and help you feel better. The top-rated specialists understand how scary bloody stools could be and come up with the best solutions to manage the underlying issues and rid of these symptoms for good.

