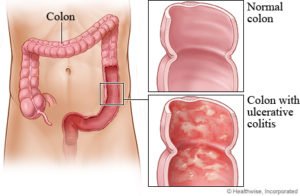
Ulcerative colitis (UC) is a medical condition that causes inflammation and ulceration in the lining of the large intestine.
Ulcerative colitis is a chronic inflammatory bowel disease that causes digestive tract inflammation. Ulcerative colitis usually affects only the lining of the large intestine (colon) and rectum. Forms range from mild to severe. It, similar to Crohn’s disease can lead to potentially life-threatening consequences.
Unlike Crohn’s disease, Ulcerative Colitis only affects the colon or the rectum, and it eats away only the innermost lining rather than eating all the way through. Ulcerative colitis causes inflammation and ulcers in the lining of your large intestine, making you feel the need to empty your bowels frequently.
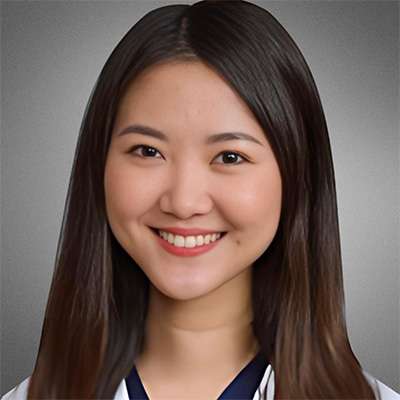
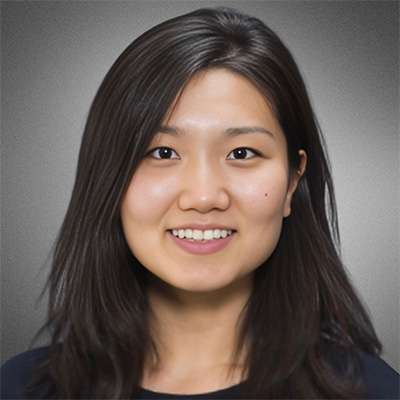
Both Ulcerative Colitis and Crohn’s disease are chronic inflammatory bowel diseases. Your symptoms may gradually worsen if left untreated. Our specialists offer expert diagnosis and treatment for ulcerative colitis in Midtown, Union Square, and Park Avenue on New York City’s Upper East Side.
Patients with ulcerative colitis are more likely to develop colon cancer. They should undergo regular screenings, which should be discussed with their local NYC ulcerative colitis treatment specialist or gastroenterologist. Fortunately, effective therapies for chronic treatment and management of this condition are now available. If you have symptoms that have previously been diagnosed as Ulcerative Colitis or are consistent with it, you should always be evaluated by a physician for an accurate diagnosis and treatment plan, as well as to establish a colon cancer screening surveillance regimen.
How Common Is Ulcerative Colitis?
Ulcerative colitis is a common condition. Together with Crohn’s disease, another form of inflammatory bowel disease, it affected about 2.5 million Americans in 2020. Experts predict that by 2030, the number of individuals living with IBD in the United States will have risen to 3.5 million.
”
★ ★ ★ ★ ★The entire staff was welcoming and made the visit quick and seamless. The office is clean, and the staff even make a point in offering coffee or water while you wait. The doctor was very friendly and to the point. Highly recommend choosing this office.
Symptoms of Ulcerative Colitis
Symptoms of Ulcerative Colitis include abdominal pain, which can be severe, and diarrhea, which can be bloody. Depending on the type of ulcerative colitis, you may also experience the following:

- Eye inflammation
- Fatigue
- A feeling of urgency
- Fever
- Joint pain
- Kidney stones
- Loss of appetite
- Osteoporosis
- Rectal bleeding
Symptoms suggestive of Ulcerative Colitis require a complete diagnostic evaluation by your gastroenterologist.
Causes of Ulcerative Colitis
Although the exact causes of Ulcerative Colitis are not known, numerous theories exist, and heredity is also an indicator. If a member of your family has Ulcerative Colitis, you are more likely to get it.
While ulcerative colitis can affect anyone, it is more common in people under the age of 30. It may also affect men more than women and affect Ashkenazi Jews more than non-Jews.
Diagnosing Ulcerative Colitis
Symptoms suggestive of Ulcerative Colitis require a complete diagnostic evaluation. Blood tests and stool samples are part of the evaluation. We will need to perform a colonoscopy to fully visualize the entirety of the colon and obtain biopsies to diagnose ulcerative colitis.
Our ulcerative colitis specialists must first rule out several other diseases such as:
- Ischemic colitis
- Irritable bowel syndrome
- Crohn’s disease
- Colon cancer
- Others that can present with similar symptoms
You should see your local ulcerative colitis specialist or our gastroenterologist establish a diagnosis and formulate your treatment plan.
Types of Ulcerative Colitis
Depending on the area of the colon affected, ulcerative colitis can be classified into several types, including:
- Ulcerative proctitis is typically the mildest type limited to the rectum (anus) and characterized by a total blurring of the normal vascular pattern and rectal bleeding.
- Left-sided colitis is found in patients in whom the inflammatory process extends up to the splenic flexure and usually leads to defecation urgency, bloody diarrhea, and associated weight loss.
- Pancolitis occurs when the entire colon is affected and results in abdominal pain, cramps, fever, blood in stool, and significant weight loss.
- Proctosigmoiditis involves the rectum and the part of the colon closest to it (sigmoid colon). Key symptoms include moderate pain on the lower left side of the abdomen, bloody diarrhea, and the inability to control bowel movements.
Manhattan Gastroenterology physicians are expertly trained and experienced in diagnosing and treating ulcerative colitis no matter the severity of disease and part of the colon affected. Get in touch with us today and start your journey to a pain-free and healthy life.
Treatments for Ulcerative Colitis
Although there is no cure for ulcerative colitis, effective therapies for chronic treatment and management of this condition are now available, which has drastically altered the disease’s natural history. Medicines, particularly biological therapies, can help reduce symptoms significantly and even provide long-term remission.
Ulcerative colitis treatment options include:
- Combination of 5 ASA drugs for anti-inflammatory properties used for mild to moderate ulcerative colitis. 5 ASA drugs provide results in 40% to 80% of patients.
- Immune system suppressors
- Biologic therapies and other modalities
Aminosalicylates are the main treatment choice for mild to moderate ulcerative colitis. You can use topical and systemic steroids to treat ulcerative colitis flares, while immunosuppressants and biological drugs can improve moderate to severe disease.
Surgery is an option if medical therapy fails. Finally, if you have Ulcerative Colitis, you should have more colon cancer screenings because you are at a higher risk of developing colon cancer. Your gastroenterologist should formulate an effective surveillance colonoscopy schedule.
Manhattan Gastroenterology’s ulcerative colitis specialists must have a broad understanding of each patient’s unique factors before devising the best treatment plan. Ulcerative Colitis is not an exception.
What Is the Best Diet for Ulcerative Colitis?
A key strategy is to maintain a healthy and balanced nutritional intake. There are no general dietary recommendations, except for the avoidance of milk and milk products for those unable to fully digest lactose. In addition, the intake of foods leading to increased stool output, such as caffeinated drinks, alcohol, red pepper, and fresh fruits and vegetables, should be reduced. During a flare-up, temporarily eating a low-residue or low-fiber diet can sometimes help improve symptoms.
Common foods to eat during a flare include non-wholegrain breakfast cereals, eggs, cooked vegetables (without stalks, seeds, and peel), white bread, lean meats, and fish. Changing your eating patterns and consuming smaller, more frequent meals can help increase the amount of nutrition you receive in a day.
Important Reminder: The only intent of this information is to provide guidance, not definitive medical advice. Please consult an ulcerative colitis doctor about your specific condition. Only trained, experienced physicians like our doctors in NYC can determine an accurate diagnosis and proper treatment.
Our doctors provide highly personalized and comprehensive care. Please contact our Union Square/Chelsea, Midtown, or Upper East Side NYC offices for more information about ulcerative colitis or to make an appointment with one of our GI specialists.