Diverticulosis Specialists
Our gastroenterologists have undergone extensive training in the evaluation of digestive diseases and are experts in the management of the diverticular disease. Our mission is to provide safe and effective therapies in a warm and welcoming environment.
What Is Diverticulosis and Diverticulitis?
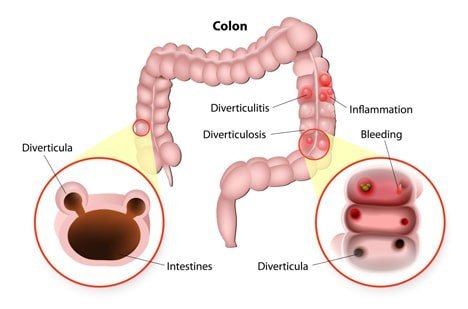
Diverticular disease, also known as diverticulosis, is a medical condition that results in the formation of tiny, pouch-like pockets in the lining of your digestive tract. Diverticula pockets can form anywhere, from your esophagus to your anus, but most commonly appear in your large intestine. They rarely cause medical problems, but they can get infected or inflamed.
Diverticulitis is caused by infection and inflammation and can lead to severe abdominal pain, nausea, and fever. In some cases, it can be a severe and life-threatening condition. If you suspect diverticulitis, you should always be evaluated with a thorough consultation and examination by the best diverticulosis doctor in NYC to ensure an accurate diagnosis and treatment plan.
How Common Is Diverticulosis?
Diverticular disease is quite common, and its incidence increases with age. It affects more than half of all Americans over the age of 60 and almost every person by the age of 80.
Who Is Most Likely to Get Diverticulosis and Diverticulitis?
Diverticulosis, however, is benign and relatively common, affecting half of all people older than 60 in the United States. Other risk factors include:
- Cigarette smoking
- Lack of exercise
- A low-fiber diet
- Obesity
It’s estimated that less than 5% of diverticulosis patients may develop diverticulitis. Common risk factors contributing to diverticulitis include:
- NSAIDs. Regular use of NSAIDs is associated with a higher risk for diverticulosis complications.
- Immune System Suppression. Certain drugs that reduce immune system activity, like steroids or immunosuppressants, can make the immune system more susceptible to infections, potentially leading to complications such as colonic perforation.
- Excessive consumption of alcohol. Those who do not drink are 2 to 3 times less likely to develop diverticulitis.
- Gender and age. Women are more likely than men to develop diverticulitis later in life.
”
★ ★ ★ ★ ★The entire staff was welcoming and made the visit quick and seamless. The office is clean, and the staff even make a point in offering coffee or water while you wait. The doctor was very friendly and to the point. Highly recommend choosing this office.
Symptoms of Diverticulosis
Most people who have diverticulosis are unaware of it. It often causes no symptoms and does not affect the digestion process.
Causes of Diverticulosis
Diverticulosis is rare when diets are high in fiber, grains, fruits, and vegetables, leading scientists and GI doctors to conclude that a low-fiber diet causes or contributes to the condition. A low-fiber diet requires additional pressure inside your digestive tract to push food along. Years of this added strain result in diverticulosis.
Diagnosing Diverticulosis
Because the majority of people with diverticulosis have no symptoms, the disease is usually discovered by accident. Diverticula can be discovered while testing for another condition with a barium enema or performing a screening exam, such as a colonoscopy. Our GI doctors recommends regular colon cancer screening once you reach 45 years of age or early, depending on risk factors. A regular colonoscopy also can detect diverticula.
Treating Diverticulosis
Diverticulosis specialists agree that the best way to treat the disease is to prevent it from happening in the first place. The way to do that is to avoid constipation by eating a diet high in fiber and rich in fruits and vegetables. Such a diet makes it easier for your digestive system to do its job, thereby preventing constipation and leading to a healthy colon.
However, once diverticula form, they do not disappear on their own. If you have diverticulosis, you will most likely don’t have symptoms or require treatment. If you do have symptoms, the first course of action is usually to increase the amount of fiber in your diet. A supplemental fiber product in pill, powder, or wafer form is an alternative treatment.
Diverticulitis is a severe condition that causes localized abdominal pain and tenderness, nausea, fever, vomiting, chills, or constipation. While our best Upper East Side diverticulosis doctors may treat a minor case with oral antibiotics, a more advanced case may require a hospital stay and intravenous antibiotics. If you have multiple cases over time, surgery to remove the affected portion of your colon may be necessary. A colonoscopy is advised after an episode of diverticulitis to rule out any underlying mass lesions. Visiting your gastroenterologist will allow them to offer you an individualized treatment plan.
When Is Surgery for Diverticulitis Considered?
Your doctor will assess various patient and disease factors before recommending surgery as the most promising treatment. These will include the likelihood of recurrence, surgical morbidity, ongoing symptoms, disease complexity, and operative risk. Admission and surgery are usually warranted in severe cases of diverticulitis, such as when the recurrent inflammation has led to the formation of fistulas or narrowing of the intestine, increasing the risk of complications.
What Does the Surgery for Diverticulitis Entail?
Surgical intervention for diverticulitis may be performed in two main ways:
- Bowel resection with primary anastomosis. This procedure involves removing the portions of the infected colon and reconnecting the healthy areas. The patient will continue to have normal digestion and bowel movements after the surgery.
- Bowel resection with colostomy. This type of surgery is used when reconnection is not possible due to high levels of inflammation. Instead, the specialist connects the healthy end of the colon to an opening made in the abdomen called a stoma. The waste will be collected in an external pouch (ostomy bag) attached to a stoma, which can be permanent or temporary.
Both procedures can be performed laparoscopically or using a traditional open technique. Laparoscopic surgery entails small cuts in the abdominal wall, cameras, and small tubes to perform the procedure, whereas open surgery requires a larger cut in your abdomen so that the specialist can view your intestines in their entirety.
Complications of Diverticulitis
Diverticulitis can develop suddenly and cause complications in about 25% of patients. The most common complications include:
- Abscess, which is a collection of infected fluid in the pouch. Abscesses are typically detected in up to 30 % of acute diverticulitis cases.
- Intestinal obstruction, which is a partial or complete blockage in the colon or small intestine due to scarring. It is rare for patients with diverticulitis to develop severe intestinal obstruction.
- Fistula, which is an abnormal connection between sections of the large intestine or the large intestine and bladder. Fistulas occur in about 14% of patients after acute diverticulitis episodes.
- Perforation, which is a rupture or tearing in the wall of the colon. Non-contained perforation occurs in 1% to 2% of acute diverticulitis patients.
- Peritonitis, which is an inflammation or infection that results from waste leaking into the abdominal lining. Peritonitis can be life-threatening and requires immediate care.
Important Reminder: The only intent of this information is to provide guidance, not definitive medical advice. Please consult a GI doctor or gastroenterology specialist about your specific condition. Only trained, experienced diverticulosis specialists like our doctors can determine an accurate diagnosis and proper treatment.
As best-in-class NYC gastroenterologists, our doctors provide highly personalized and comprehensive care. For more information about Diverticular Disease or to schedule an appointment with one of our GI doctors, please contact our Union Square/Chelsea, Upper East Side, or Midtown NYC offices.

